For many patients with cancer today, treatment success can be difficult to define. Oncologists may recommend and deliver multiple rounds of potentially life-saving treatments without knowing if each one is truly doing its job.
“We don’t know if chemotherapy, in particular, successfully damages the patient’s cancer after a single dose,” said Brandon Mancini,MD, MBA, FACRO, Medical Director at BAMF Health. “We have a high degree of confidence, but we commonly can’t tell patients after cycle one or two whether their tumors are responding to the prescribed treatment. Most often, we must wait several cycles to quantify the impact of therapy.”

Patients may continue to receive their planned cycles of chemotherapy even if the cancer drastically responds to initial treatments. At that point, normal tissues could be irreversibly damaged. Dr. Mancini and the team at BAMF Health believe patients deserve more certainty.
Radiopharmaceutical Therapy vs. Chemotherapy
Radiopharmaceutical therapy is emerging as a promising treatment for cancer patients. While there are currently only two FDA-approved therapies for prostate cancer and neuroendocrine tumors (NETs), dozens of drugs that treat other cancers are in the clinical trial pipeline.
Lutetium Lu177 vipivotide tetraxetan is approved for the treatment of adults with PSMA-positive metastatic castration-resistant prostate cancer. Lutetium Lu177 dotatate is approved for the treatment of adults and children aged 12 years and older with gastroenteropancreatic neuroendocrine tumors (GEP-NETs).
Dr. Mancini explains that Lu177 is an IV injection that emits therapeutic radiation (i.e., high-energy beta particles) to damage cancer DNA. This radiation has little, if any, impact on surrounding normal tissue because it attaches to specific markers found primarily on the cancer cells being targeted. The treatment delivers very focused and specific radiation.
“Chemotherapy, while extremely effective and the only option for some patients, is far less specific. It is cytotoxic to cancer cells, but normal tissues are more greatly impacted,” Dr. Mancini added.
The TheraP study published in 2021, compared men with metastatic castration-resistant prostate cancer treated with LuPSMA to those treated with second-line cabazitaxel chemotherapy. The results revealed those treated with LuPSMA had a higher PSA response and fewer adverse events.
Integrating SPECT/CT Into Therapy Protocols
Dr. Mancini and the team at BAMF Health have experience delivering thousands of radiopharmaceutical therapy doses. As a result, they’ve developed a unique protocol for giving patients critical feedback after each therapy dose.
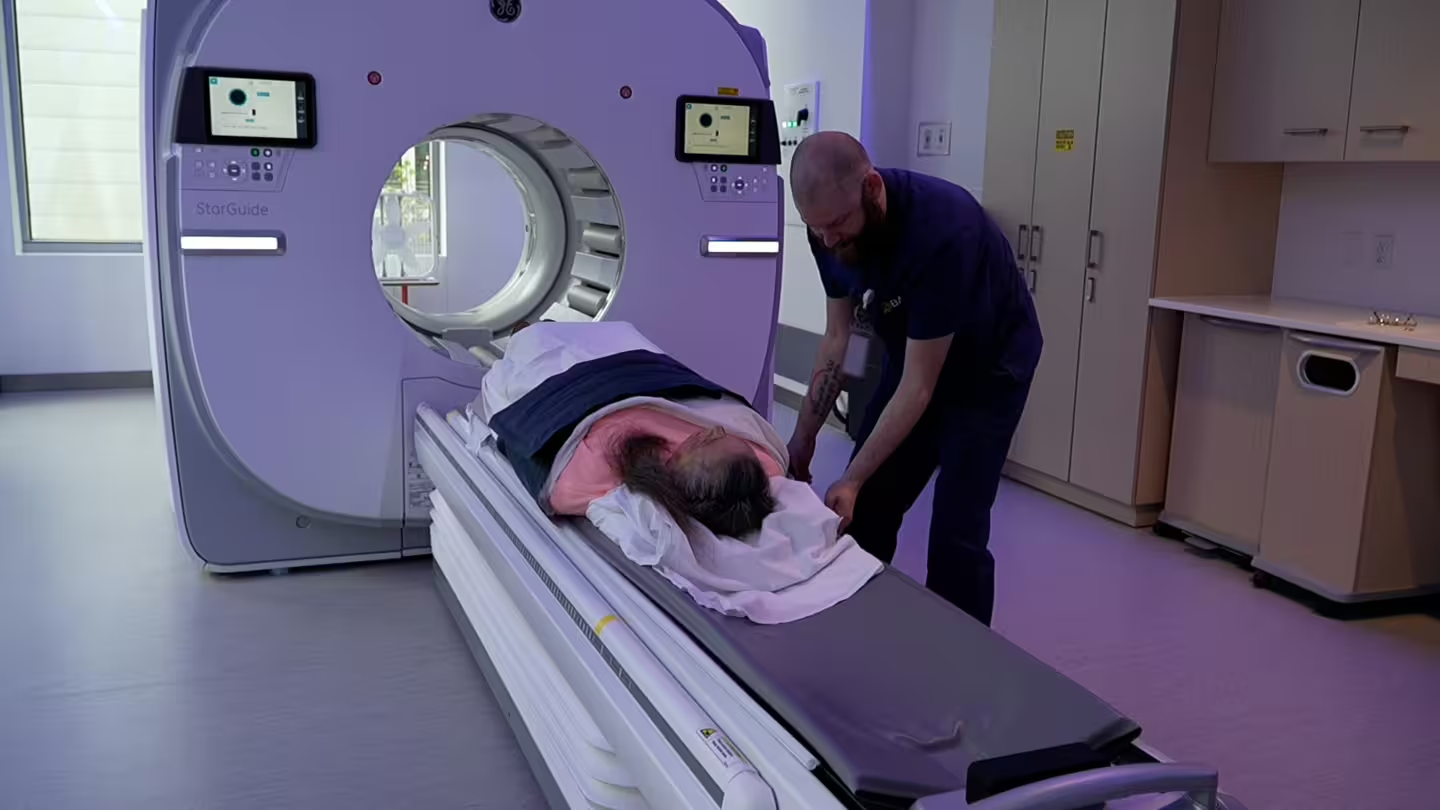
This is accomplished through post-therapy SPECT/CT imaging and consultation. BAMF Health was the second site in the U.S. to install GE HealthCare’s most advanced digital SPECT/CT, StarGuide™.

“GE HealthCare designed our StarGuide SPECT/CT system to provide clinicians with the data they need to help them make personalized care decisions and treatment recommendations,” said Chris Heble, Senior Director, U.S. and Canada Molecular Imaging Strategy, GE HealthCare.
StarGuide captures gamma rays emanating from tumors after therapy injection. The approximately 20-minute SPECT/CT scan localizes and quantifies drug uptake in the patient’s body.
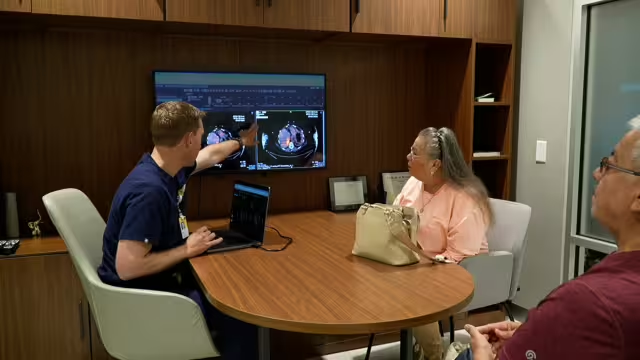
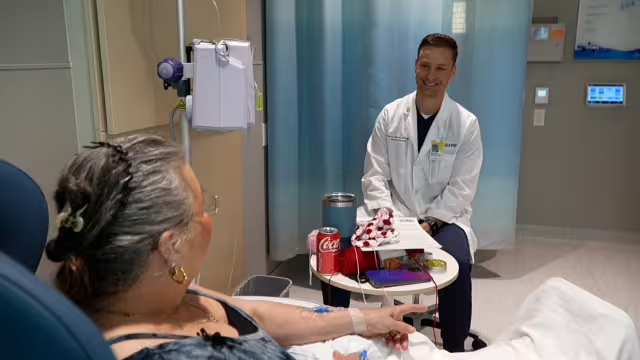
Not every treatment center uses SPECT/CT, but Dr. Mancini views it as BAMF Health’s superpower. “Treatment is no longer a guessing game because we leverage the results from our patients’ SPECT/CT scans to personalize therapeutic decisions,” he said. “We give patients a scan approximately 24 hours post-therapy and immediately sit down to discuss the results with them. This gives them instant feedback about where the drug has accumulated, how much has accumulated, and how the size and distribution of their tumors have changed.”
The Value of SPECT/CT for Patients
Dr. Mancini says patients are empowered by the SPECT/CT results. It reduces anxiety and decreases the psychological stress of waiting weeks or even months for answers.
In some cases, the results are so promising, patients can temporarily postpone further cycles of radiopharmaceutical therapy. This means they avoid unnecessary radiation, and the overall costs to patients and the health system in general decreases.
“We are only just beginning to realize the potential of SPECT/CT,” said Dr. Mancini. “This technology will continue to advance and allow for further personalization of therapy for patients. The future of cancer treatment is precision medicine, and BAMF Health is leading the way.”
“StarGuide aims to help fulfill the promise of nuclear medicine’s Theranostics revolution,” said Heble. “We believe it’s a future-proof breakthrough that will help expand the horizon of personalized treatment and transform Theranostics imaging innovation forever.”


